Prior Authorization (PA) is required for nearly all specialty products and is largely responsible for delayed patient initiation. Lengthy PA delays can ultimately result in cancellations for new patient referrals, adherence/persistence problems, and lower patient satisfaction.
There are several ways specialty brands can improve patient initiation by implementing data-driven patient support strategies (See Figure 1). Successful interventions to streamline patient initiation have the potential to speed Time to First Fill and increase overall Fill Rate for new patient referrals.
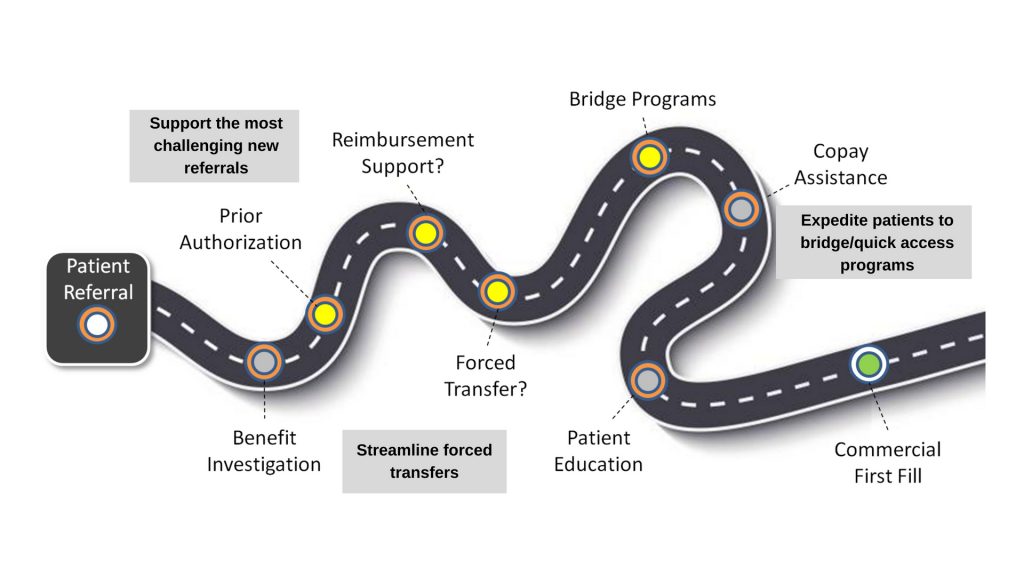
Figure 1: Key Opportunities to Improve Patient Initiation
Each key opportunity to improve patient initiation is related to a friction point in patient access. This post provides an overview of these key opportunities and the potential of analytics to unlock efficiencies for specialty brands.
Support the Most Challenging New Patient Referrals
If the most challenging new patient referrals were triaged to field reimbursement or hub support earlier, specialty brands could improve average Time to First Fill and reduce cancellations.
The first step in prioritizing at-risk patient cases (those that have stalled in PA) for reimbursement support services is filtering out the noise in patient sub-status data. Cleansed, granular data creates visibility into patient access steps from initial referral to PA to active ship. Processes to improve the quality of specialty pharmacy data include the clean up of missing and inaccurate sub-status records and enrichment of the sub-status information.
Next, specialty brands need to establish a baseline for measurement.
Measure Time Spent in Prior Authorization
Calculating the average time spent in the PA step across a network of specialty pharmacies is another important capability for identifying and triaging the most at-risk patient cases. A network average for baseline metrics such as Time to First Fill and Fill Rate allows specialty brands to evaluate performance of their contracted SPs and provide coaching in an SP account review setting.
In this example, the percentage of new patients that are experiencing PA delays for a specific threshold (5 days) is calculated to identify the most at-risk patients. (Figure 2) What happened to those patients and what type of support services were offered to help them start on therapy?

Figure 2: Analysis of patients stalled in prior authorization
Based on the stalled PA analysis, account managers can coach SPs to ensure sub-status reporting meets contract specifications and that the most high-priority cases are being triaged to the hub or otherwise supported.
Streamline Forced Transfers
New patient referrals, and in some instances refills, are often forced to transfer from one specialty pharmacy (SP) to another. Why? Exclusive specialty networks, which are largely enforced by a handful of Payers and Pharmacy Benefit Managers (PBMs), limit the number of entities that can fill a script.
Specialty manufacturers want these high-risk patient referrals quickly triaged and routed to reimbursement services. If not addressed, forced transfers can delay therapy initiation, increase average Time to First Fill, and lead to higher abandonment rates.
Forced transfer analytics calculate the percentage of patients being referred that are unlikely to fill at a given SP. The opportunity is educational. Specialty brand account managers now have the data to make a case for greater urgency when SPs encounter a script that should be transferred. Health care providers (HCPs) should also be made aware that patient referrals to this SP are unlikely to be filled for certain prescriptions.
Expedite Eligible Patients to Bridge/Quick Access Programs
The high cost of specialty medications and considerable policy restrictions are obstacles for patients attempting to access life-saving therapies in a timely manner. To help patients navigate these obstacles, pharmaceutical manufacturers offer solutions such as bridge supply/quick access programs. These courtesy prescriptions help patients start therapy sooner while coverage issues are resolved. For specialty brands to effectively and efficiently use bridge, they need to identify eligible patients (patients whose pharmacy or medical benefits will ultimately be approved) and connect them to the bridge fill faster.
Patient cases that are slow to initiate a bridge program are likely experiencing a PA delay. Specialty pharmacies are often reluctant to triage the patient case to reimbursement services for fear the patient will be transferred back to complete the first commercial fill.
Bridge analytics calculate the average time from patient referral to bridge initiation and Fill Rate for patients delayed for a specific threshold with no bridge fill. Poor performance in these areas represents a coaching opportunity for SPs.
Conclusion: How to Improve Patient Initiation
If properly analyzed and acted on, the three key opportunities to improve therapy initiation with data-driven patient support can lead to better outcomes. Patients who would have never been identified as at-risk due to stalled PA and forced transfers will be prioritized for reimbursement support, improving a brand’s key metrics such as Time to First Fill and Fill Rate.
Of course, the quality of sub-status data is critical to success. Missing and incorrect information will impair a specialty brand’s ability to analyze patient access steps and gain insights.
Lastly, the analytics described here and resulting actions are reactive. Predictive and prescriptive analytics related to the three key opportunities have the potential to create an even greater impact on patient initiation.
About the Author
Sean McCarthy brings a unique background to IntegriChain with over 20 years of experience worked in both pharmaceuticals and the technology provider space. Sean, who most recently served as Director, Market Access Strategic Planning at Boehringer Ingelheim, has spent time at Veeva Systems and Model N. At IntegriChain, Sean will lead the development of the company’s specialty analytics and specialty data aggregation offerings as the Segment Leader, Patient Access.






